Systematic Development of Evidence-Based Faculty and Student Medication Calculation Knowledge, Skills, and Attitudes through Asynchronous Electronic Media
|
Linda J. Porter-Wenzlaff
Clinical Associate Professor/Distinguished Teaching Professor
School of Nursing
The University of Texas Health Science Center at San Antonio
porterl@uthscsa.edu
Janis N. Rice
Clinical Associate Professor/Distinguished Teaching Professor
School of Nursing
The University of Texas Health Science Center at San Antonio
ricej@uthscsa.edu
Lisa M. Sievers
Clinical Instructor
School of Nursing
The University of Texas Health Science Center at San Antonio
sieversl@uthscsa.edu
Abstract
In response to the Institute of Medicine's focus on adverse events, fatal medication errors, and Quality and Safety Education for Nurses (QSEN) competencies, best educational practices and current technology were applied within a knowledge translation model to embed a single consistent, evidence-supported medication calculation process, dimensional analysis (DA), across the undergraduate nursing curriculum at the authors' institution. Rosswurm and Larrabee's (1999) conceptual model for change to evidence-based practice guided the implementation process. Beginning in May 2010, four self-paced online DA modules developed on Sonic Foundry's Mediasite webcasting platform using a problem-based format were incorporated into a continuing education packet to build foundational faculty competency and teaching consistency, and to serve as a basis for classroom education and ongoing student remediation. Impact surveys were conducted April 2011 following three semesters of use. Consistent application and reinforcement of the DA strategy has resulted in student and faculty reports of greater student calculation competency and confidence, which will potentially translate into increased patient safety in practice.
Keywords: dimensional analysis (DA), nursing education, Quality and Safety Education for Nurses (QSEN), Sonic Foundry, Mediasite, webcasting, web-based learning modules, change management, knowledge translation model, system competency, culture of safety |
Introduction
The Institute of Medicine (IOM, 2006) reports that 41% of fatal medication errors are the result of medication administration errors. In a 2006 study of 229 second-year nursing students and 44 registered nurses, McMullan, Jones, and Lea (2010) found that 92% of the students and 89% of the registered nurses failed a calculation test, and that 55% of the students and 45% of the registered nurses failed a numeracy test. The concern for accurate calculation competency and the IOM's ongoing focus on adverse events and fatal medication errors, coupled with the introduction of the Quality and Safety Education for Nurses (QSEN, 2011) competency standards, challenge schools of nursing to identify and teach best medication calculation and administration practices. The use of best educational practices is also needed to ensure student learning and thus positive client outcomes within a culture of safety. The formation of students' medication calculation and administration knowledge, skills, and attitudes is founded in a robust and well-structured curriculum, effective teaching strategies, clinical reinforcement, and faculty modeling. While the work reported in the present paper focuses specifically on calculation competencies, it is set within the context of the full scope of actions and considerations related to medication administration. Strong student calculation competency is but one of the ingredients required for the achievement of positive patient outcomes. Current technology affords the ability to ensure ongoing access to consistent information for all faculty and students, supporting adult education principles related to the timing of learning proximal to the need to know, and facilitating ongoing reinforcement and remediation. However, establishing one consistent best practice across a large school and multi-track curriculum encompassing all faculty, simulation and skills lab staff, and students is challenging and calls for purposeful, system-wide planning and coordination. Thus, use of a structured model for translating evidence into practice is desirable.
Dimensional analysis (DA) has been identified as a best calculation practice (Craig, 1997; Greenfield, Whelan, & Cohn, 2006; Rice & Bell, 2005) when compared with commonly used ratio-proportion equations. A decision was made to implement DA throughout the undergraduate nursing program at The University of Texas Health Science Center at San Antonio (UTHSCSA). Implementation in this large program commenced with faculty, to ensure their competence and reinforce the use of one consistent process before it was extended to students. Four self-paced, problem-centered web-based learning modules were developed, with online problem-based exercises to gather evidence of competency. Rosswurm and Larrabee's (1999) conceptual model for change to evidence-based practice guided the implementation. This paper provides an account of the process and experiences, and presents student- and faculty-reported outcomes. Areas for further development and study are discussed.
Literature Survey and Best Practices
Medication Error Rates and Consequences
An IOM (2006) report identified medication errors as being among the most common medical errors, harming at least 1.5 million people every year. Medication errors alone account for an estimated 7,000 deaths annually (Brennan et al., 1991; Thomas et al., 1999). The extra medical costs of treating drug-related injuries occurring in hospitals alone conservatively amount to $3.5 billion a year. Although error rates vary widely across facilities, the IOM (2006) estimates there is at least one medication error per hospital patient each day. In a study by the U.S. Food and Drug Administration that evaluated reports of fatal medication errors during the six-year period from 1993 to 1998 (Phillips et al., 2001), it was found that the most common error involving medications was related to administration of an improper dose of medicine.
A recent retrospective study of client records from 2002 to 2007 across 10 North Carolina hospitals again revealed medication errors were one of the most common causes of all medical errors for hospitalized patients (Landrigan et al., 2010). That study also addressed the lack of statistically significant change in the rate of preventable harms per 1,000 patient days over the six-year period with which the study was concerned. In a review of 33 articles addressing medication errors, Wright (2010) found only five that specifically recorded information related to calculation errors, and only two that detected calculation errors using direct observation. In this literature review there were no articles found that related directly to nurses' lack of calculation competence leading to actual medication errors. This is reflective of the motivation driving the current impetus to look at the overall process of medication administration across the inter-professional healthcare team.
The IOM has provided recommendations to enhance medication safety by establishing "explicit performance standards for patient safety through regulatory and related mechanisms, such as licensing, certification, and accreditation," recognizing that these can "define minimum performance levels for health professionals, the organizations in which they work, and the tools (drugs and devices) they use to care for patients" (Kohn, Corrigan, & Donaldson, 1999, p. 4). The IOM further suggests that a culture of safety can be cultivated by designing jobs and working conditions focused on safety; standardizing and simplifying equipment, supplies, and processes; and avoiding the need for care providers to rely on memory.
Establishing an environment that systematically and intrinsically demonstrates value for patient safety by addressing standardized minimum performance levels, evidence-based processes, and decreased reliance on memory was determined by the faculty at the UTHSCSA School of Nursing to be critical in fostering a culture of safety in the education of registered nurses relative to medication administration. The calculation problems used across the School's courses and in simulation and clinical are framed to build and assess students' conceptual understanding of the clinical problems presented. Clinical and simulation experiences address the technical aspects of delivery, while professional role development establishes accountability for a practiced culture of safety. It is this combination of knowledge, skills, and attitudes that affords the desired client outcome, with each component needing rigorous development.
Best Practice: Evidence-Based DA Calculation Process
In episodic discussions within the UTHSCSA School of Nursing's Committee on Undergraduate Studies (COUS) and various team meetings between 2000 and 2009 faculty expressed concern about inconsistent student calculation competencies ascribed to basic mathematical errors, including reliance on mental math, inaccurate conversions, transposition errors, inaccurate formula application, nervousness, insecurity, and hurried work. Various previous attempts made by faculty to enhance performance had been ineffective in fully resolving competency gaps. It became apparent that a systematic, evidence-based approach to medication calculations was required to maximize student competency outcomes. In response, DA was explored by a core faculty group and concluded to be an evidence-supported best practice methodology that would lend itself to enhanced student calculation competence.
Figure 1 demonstrates two medication calculations using DA. Evidence attests to the fact that DA is superior to ratio proportion in assuring calculation accuracy (Craig, 1997; Greenfield et al., 2006; Rice & Bell, 2005). Boucher (2007) points out that DA uses the same steps for every calculation, removing the necessity for students to learn or use multiple approaches. Greenfield et al. completed a pilot study that evaluated if using DA could reduce calculation errors. The scores of students using DA in a medication calculation examination were compared with those of students using the traditional formula memorization method. The control group's scores on the examination ranged from 46 to 100 (mean = 86.92, SD = 14.5). With the passing score set at 90, 16 of the 26 students (61.5%) passed using traditional methods and 10 (38.5%) failed. The experimental group's scores ranged from 75 to 100 (mean = 92.12, SD = 6.2); 33 of the 39 students in that group (84.6%) passed, with only 6 (15.4%) failing (Greenfield et al., 2006). Results therefore signaled that the DA group achieved greater accuracy and made fewer calculation errors than the traditional-math group.
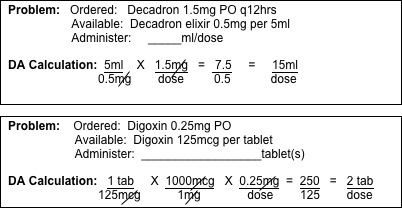
Figure 1. Two DA medication calculation examples
Craig (1997) reports nursing students identified that DA was an effective problem-solving method for medication calculations that assisted them in improving mathematical, conceptual, and cognitive skills, and in addition lowered their anxiety levels. Because of the ability to be visualized and followed in a logical manner, DA was found to be effective for both right-brain and left-brain learners. All of the nursing students (100%) in Craig's study strongly agreed or agreed that DA improved their mathematical calculation and conceptual abilities, with 92% strongly agreeing or agreeing it improved their cognitive abilities, and 77.8% strongly agreeing or agreeing it reduced their anxiety when solving medication calculation problems. This decrease in anxiety and increase in confidence were deemed critical in building calculation competency that would transfer into practice upon graduation. In a survey conducted by the American Nurses Association (2007), it was found the overwhelming majority of U.S. nurses (97%) worry about medication administration errors, and nearly all (99%) believe there is a grave risk to patients when errors occur. The Association also discovered the errors are most likely to occur during preparation and administration of medication (48%) and in the transcription of initial orders (47%).
At the UTHSCSA School of Nursing, the available evidence pointed strongly to the fact DA would boost both accuracy in all medication calculation situations as well as student self-efficacy and confidence in those situations. A survey of current students revealed that, unlike faculty – who had primarily learned and were using ratio proportion – students now routinely learned DA in middle and high school as well as in pre-requisite chemistry courses. Use of DA in their undergraduate nursing courses would therefore build on their prior knowledge. Once DA had been identified as the best calculation practice, an analysis of its fit with QSEN's competencies and of the processes that could be used to enhance its implementation at the School followed.
Building a Culture of Safety: Quality and Safety Education for Nurses (QSEN)
QSEN addresses the need for effective use of strategies and technology by nurses to lower their reliance on memory and to reduce their risk of harm to themselves, their patients, and others with whom they are working (Greiner & Knebel, 2003). The QSEN (2011) competencies stipulate consistent use of evidence-based processes in order to maximize outcomes. Faculty supporting DA adoption were aware that various medication calculation processes were being taught across the two BSN curriculum tracks, and that students often struggled with more complex calculation problems. The dissonance in student and faculty calculation processes based on educational backgrounds was acknowledged. Lack of a basic safety design principle, inconsistently applied calculation processes, and sub-optimal pedagogical strategies allowed potentially unsafe practice skills to develop. It was recognized that consistent use of DA across the curriculum, together with faculty modeling and other instructional strategies to support ongoing and increasingly complex calculations, would be in line with and assist in the attainment of the safety-related knowledge, skills, and attitudes defined in the QSEN safety competencies. Discussions within COUS echoed the need for deliberate, consistent, ongoing formative and summative evaluation of calculation competencies across the curriculum.
As stated, the QSEN competencies set out the knowledge, skills, and attitudes that nurses need to develop in relation to practice safety. Consistent systematic use of DA for medication calculations addresses each of these components. The QSEN knowledge competencies include, for example, awareness of human factors and other basic safety design principles, as well as common unsafe practices (e.g., workarounds and dangerous abbreviations); understanding of the benefits and limitations of selected safety-enhancing technologies (e.g., barcodes, computer order entry, medication pumps, automatic alerts/alarms); and familiarity with strategies for reducing reliance on memory (QSEN, 2011, "Safety" section). Consistent use of DA provides a basic safety work design shown by evidence to decrease human error. Among the QSEN skills competencies are demonstrating effective use of technology and standardized practices that support safety and quality; demonstrating effective use of strategies to reduce risk of harm to self or others; and using appropriate strategies to reduce reliance on memory (e.g., checklists) (QSEN, 2011, "Safety" section). DA is especially suitable here as it does not depend on memory or recall of equations in order to accomplish accurate calculations. The QSEN attitudes have to do with qualities such as valuing the contributions of standardization/reliability to safety; appreciating the cognitive and physical limits of human performance; and recognizing one's own role in preventing errors (QSEN, 2011, "Safety" section). The results and observations from the implementation of DA at the UTHSCSA School of Nursing support the literature advocating DA as a more effective calculation method. Systematic education and universal use of DA across the curriculum has highlighted the value for faculty in using evidence to drive practices that reduce the potential for patient harm.
Best Educational Practices
In an effort to optimize learning, best practices in online learning (Billings & Connors, n.d.) were reviewed, and implementation planned based on adult education principles (Billings & Halstead, 2009) and with the help of Rosswurm and Larrabee's (1999) six-phase model for translating evidence into practice. Four web-based learning modules were developed that teach theory relating to DA, followed by step-by-step demonstration of its application to multiple calculation problems, allowing learners to work along with the demonstration. Table 1 outlines the content and distribution of the modules, which build progressively from simple to complex.
Sonic Foundry's Mediasite webcasting technology was used to produce the learning modules. Mediasite allows for the streaming of an audio-visual lecture with synchronized PowerPoint or overhead visuals on one split screen. Figure 2 is a screen capture of a DA calculation step being presented on Mediasite, with the video feed of the instructor on the left and an overhead showing progressive problem work on the right.
Table 1. DA modules product
Module |
Content |
Distribution |
Module 1:
Using DA to Calculate Drug Dosages and Rate of Administration
|
- Four areas of concern:
- Conceptual
- Conversion
- Calculation
- Critical Thinking
- Introduction to DA
- Steps in DA
- Examples of DA
|
Semesters 1, 2, 3, 4:
Traditional students
Accelerated students
Faculty CEU
RN refresher course
Continuously online |
Module 2:
Applying for PO, IM Drugs
|
- PO, IM DA calculations
- 15 problems worked step by step
|
Semesters 1, 2, 3, 4:
Traditional students
Accelerated students
Faculty CEU
RN refresher course
Continuously online |
Module 3:
Using DA for IV, IVPB, IV Drips
|
- IV, IVPB, IV drips DA calculations
- 17 problems worked step by step
|
Semesters 2, 3, 4:
Traditional students
Accelerated students
Faculty CEU
RN refresher course
Continuously online |
Module 4:
Using DA for Pediatric Clients
|
- Pediatric DA
- Common conversions
- 15 problems worked step by step
|
Semesters 3, 4:
Traditional students
Accelerated students
Faculty CEU
RN refresher course
Continuously online |
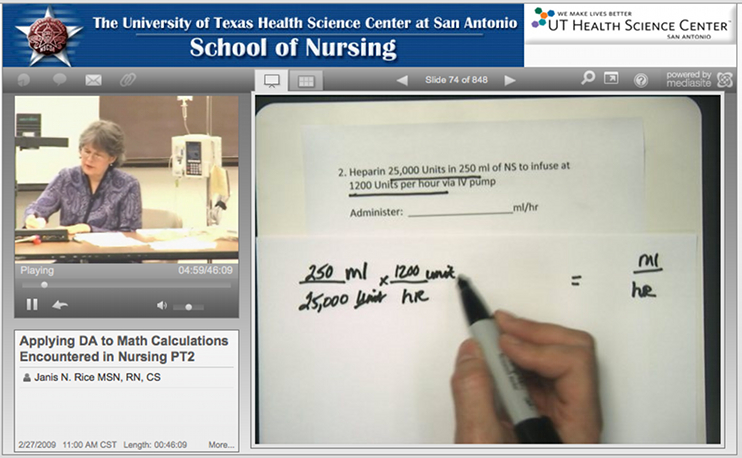
Figure 2. Snapshot of the in-world classroom
Because the web modules are continuously online, faculty and students can access them on demand at any time to cater to their need for flexible, "just-in-time" learning and revision. The modules are first presented to students formally as part of targeted courses across semesters, with the additional support of an initial, dedicated face-to-face session in first semester. Learning is promoted through class work, clinical application, and formal examinations. These strategies collectively accommodate multiple learning styles, including auditory, visual, and kinesthetic (Fleming & Mills, 1992), as well as converger, diverger, assimilator, and accommodator processes (Kolb, 1984). Students having difficulty or in need of additional time may independently refer to the modules as necessary, and moreover may seek assistance from faculty and peers. An important benefit of the DA modules is method standardization so that everyone utilizes one consistent, evidence-supported method. The same modules were used to provide the continuing education unit (CEU) program for faculty, minimizing confusion and maximizing opportunities to encourage competence bulding and "buy in."
Knowledge Translation Model Application
According to the Agency for Healthcare Research and Quality (AHRQ, 2001), "Translation of research findings into sustainable improvements in clinical outcomes and patient outcomes remains a substantial obstacle to improving the quality of care" (para. 1). The evidence suggests that it may take as many as two decades for research outcomes to become a routine part of clinical practice (AHRQ, 2001). In a review of published studies evaluating the quality of American healthcare, it as found that only three out of every five chronically ill patients received the recommended care (Schuster, McGlynn, & Brook, 1998). While more recent research is beginning to show successful translation is taking place episodically, it is largely context specific, and what works in one situation may not readily transfer to another (AHRQ, 2001). It was thus acknowledged that it would be challenging to effect timely, system-wide change across the large undergraduate nursing program at UTHSCSA to achieve consistent use of the evidence-based calculation method by all faculty and students. In recognition of the fact that change in current practice is difficult to accomplish, a deliberate and defined model, that proposed by Rosswurm and Larrabee's (1999), was chosen to guide the incorporation of DA into the curriculum. The six phases that have been followed in line with this model are described below.
Phase 1: Assess the Need for Change in Practice
The IOM's (2006) agenda of pushing for continuous improvement in medication administration safety has led nurses in all areas of education and practice to assess their related processes and outcomes. At the UTHSCSA School of Nursing, the sporadic initiatives aimed at enhancing performance that had been driven by faculty working together on COUS and in smaller course teams in the past had been ineffective in terms of fully mitigating competency gaps. Stopping to seriously and thoroughly reflect on current educational practices and student outcomes led to a clear mandate for concerted action.
Phase 2: Link the Problem with Interventions and Outcomes
Approximately 14 years prior to the formal initiation of the move to adopt DA as standard practice at the School, a few faculty – including one of the authors of this work – began to explore the literature and to build personal competency in DA. Over the intervening years, with the guidance of these pioneering faculty several additional faculty individually converted the calculation expectations in their courses to DA, realizing it to be a superior process leading to enhanced student outcomes. Collective experiences and the evidence presented by the DA faculty champion at committee meetings served as strong indicators of the existence of the opportunity to improve competencies.
Phase 3: Synthesize the Best Evidence
In order to establish a comprehensive understanding of best evidence and the best approach to achieving change, a comprehensive literature review was carried out. This literature review covered the use of DA, nursing medication errors, models for successful evidence translation, and evaluation of QSEN competencies and strategies within a best educational practices framework.
Phase 4: Design a Change in Practice
Based on QSEN (Cronenwett et al., 2007) and the 2008 Essentials of Baccalaureate Education published by the American Association of Colleges of Nursing (AACN, 2008), the BSN curriculum was revised over 2008 and 2009 for 2010 implementation. This provided an opportunity for systemic change to be considered as an integral part of an enhanced focus on safety. The DA implementation plan was defined within COUS and endorsed in March 2010.
Evaluation
Phase 5: Implement and Evaluate the Practice
Four learner-paced, problem-centered web-based learning modules on DA were produced on Mediasite, as described earlier. All undergraduate faculty and Learning Lab staff were given an online CEU packet (4.5 CEU credits) and four months (May 2010 to August 2010) in which to complete the modules and related exercises to demonstrate baseline competency. Three faculty DA champions made themselves available as mentors. Faculty completion was tracked and periodic reminders sent to those who had yet to complete the modules. By the end of August 2010, approximately 25% of the designated faculty had completed the packet. The need for faculty to "teach out" the remaining offerings of the outgoing curriculum while simultaneously developing and teaching the new curriculum imposed additional workload and increased stress. This was an opportune time to integrate DA into the new curriculum, but it was not an ideal time for faculty to have to learn a new method of calculation. Emphasis was placed on faculty initiating the new curriculum in Fall 2010, while others were asked to complete the modules by the end of the year. With ongoing tracking and reminders, by the end of the Fall 2010 semester approximately 70% of faculty had completed the modules. Department Chair support was sought and time dedicated during department meetings to assist in raising completion rates. By May 2011, 90% of faculty and all Learning Lab staff had completed the modules.
The online modules and face-to-face reinforcement were initiated with incoming accelerated Semester 1 students in June 2010 and traditional Semester 1 students in September 2010. DA continued to be implemented through Fall 2010 and Spring 2011 semesters, with three semesters of accelerated student exposure and two semesters of traditional student exposure occurring by May 2011. Reinforcement took place face to face in class and clinical. Ongoing calculation problems were used across courses within their examination structures to challenge students to attain and sustain competency. Survey evaluations of student and faculty experiences and outcomes with DA as well as of usage and effectiveness of the modules were conducted in late April 2011; an overview of the results is displayed in Tables 2 and 3.
Table 3. Survey DA survey results
Survey Item |
Percent of Student Response
(N = 128) |
Traditional students who learned DA prior to nursing school
|
97.6 |
| Traditional students who plan to use DA in practice |
97.7 |
| Second-degree students who learned DA prior to nursing school |
73.0 |
| Second-degree students who plan to use DA in practice |
66.6 |
| Confidence in DA calculations (at a score of 8-10 on a 10-point scale) for all students halfway through the undergraduate BSN Program |
62.0-66.0 |
| All students reporting their calculation accuracy is at 90% or better |
80.6-85.5 |
| All students reporting the DA modules as helpful or very helpful |
66.0-82.0 |
Table 3. Faculty DA survey results
Survey Item |
Percent of Student Response
(N = 128) |
Faculty with no prior DA experience
|
50.0 |
| Faculty who have confidence in DA calculations (at a score of 8-10 on a 10-point scale) |
72.7 |
| Faculty reporting the DA modules as very helpful |
78.6 |
| Faculty reporting use of DA for student calculations and teaching it in the classroom and clinical |
79.0 |
| Faculty using the DA modules for student remediation |
63.0 |
| Faculty believing DA decreases medication calculation errors |
63.0 |
| Faculty believing students now achieve 90% or better accuracy with calculations using DA |
75.0 |
Lessons learned and future improvement actions were addressed through COUS in May 2011 (Table 4).
Table 4. Lessons learned
- Establish a clear definition of competency expected as well as quantified related evidence of needs and the benefits anticipated at the onset of the plan.
- Clearly explore all system issues related to the project at the onset of the plan and identify needed strategies to address them, including key players.
- Establish a clear, comprehensive operational plan with benchmarks for processes and outcomes, and define formative and summative evaluation time points and reporting mechanisms.
- Identify all associated costs and funding sources at the onset of the plan.
- Discuss competency standards to gain support as well as to identify all potential curriculum, program, and accreditation issues with Department Chairs and Associate Deans prior to establishing criteria.
- Clearly identify who should be included and who might be waived from criteria accountability and engagement prior to initiating the change, and support decisions with rationale.
- Establish clear and reasonable timelines for attaining faculty competency with related accountability.
- Establish clear tracking and competency documentation/reporting processes at the onset of the plan for students and for faculty.
- Sustain a standing committee agenda item and assure time for discussions related to formative and summative data, problem solving, process improvement, and plan refinement.
- Punctuate successes!
|
Discussion
Phase 6: Integrate and Maintain the Practice Change
Integration continues; it is well known that fully translating evidence into practice often takes many years. Blank, Tobin, Macomber, Jaouen, Dinola, and Visintainer (2009) studied medication errors in an emergency department and found 36% were made in the medication administration phase. They conducted a three-month education intervention. Pre-test scores were 69% correct, while post-test scores increased to 91% correct. However, when they assessed changes in error rates post intervention, they found only a 1% decrease. This reflects the need to look at each step in the entire medication delivery process, both individually and holistically, in order to improve safety, and also suggests that knowledge acquisition does not necessarily always lead to changes in practice behavior. By May 2011, all targeted faculty had completed the DA learning modules, but there are faculty in clinical courses that do not allow students to administer medications, and faculty teaching didactic courses who have questioned the necessity of learning and/or incorporating DA problems into their course and assessment processes. There are also faculty who have successfully used ratio proportion throughout their careers and who are apprehensive or resistant toward switching to a new, less familiar process. They admit they may not use DA consistently in clinical practice themselves, and do not focus on consistent use of DA with students in their courses. Resistance to change is a multifaceted reality, as are faculty turnover and use of faculty extenders. The authors believe the systemic change they are engaged in will necessitate and demand ongoing facilitation. Additional outreach will be needed to include and incorporate dedicated education unit lead teachers, emersion preceptors, and adjunct faculty.
This experience has nevertheless been a productive step toward a fully engaged, evidence-based practice change. Student evaluation data support continued use of the modules with the addition of further practice opportunities. Additional content development for independent student study is planned. COUS recommendations arising from the student evaluation data include increased emphasis on safety-driven processes to enhance student focus on an attitude of safety, moving from task completion to an appreciation of medication administration as a therapeutic intervention with substantive consequences.
Calculation accuracy is only one component of a complex and dynamic process that students must attend to when administering medications. As such, this experience has highlighted the need to strengthen the curriculum to enhance students' understanding in a number of areas, including populations (geriatric and pediatric) and situations (emergency responses) of increased vulnerability for errors; Joint Commission standards supporting safety (list of abbreviations that should not be used); levels of institutional prevention (computer physician order entry, clinical pharmacist engagement, barcoding); and current trends in nursing to strengthen medication delivery safety (use of signage or orange vests to support a singular focus on medication delivery, accurate patient weight policies, addressing medications that are similar in appearance, dealing with high-alert medications). (Leonard, 2010; Schlesselman, 2011).
Evaluation data from faculty employing DA are very telling of significant progress in the establishment of faculty competence and the integration of DA throughout the BSN curriculum. Faculty engagement is improving, and there is a sustaining commitment to teaching and using DA. COUS recommendations relating to faculty include ongoing work to engage all faculty, continued faculty competency development, increasing opportunities for student practice with complex problems, and benchmarking for ongoing confidence and calculation competency improvement. The Department Chairs have incorporated DA faculty competency tracking through annual performance evaluations, and have added the module packet to the orientation for new faculty.
Conclusion and Future Plans
Areas flagged for further consideration include the possibility of providing students with access to additional DA calculation problems for enhanced self-directed learning and continuing application remediation, as well as an increased focus on building strengthened safety value formation in students for the overall process of medication delivery. Ongoing minimum benchmarks for calculation competency at identified points across the curriculum, together with clear action plans for outliers based on national and School data, need to be established. Due to the potential for patient harm related to calculation errors, the target benchmark to be reached is ultimately 100% accuracy. There can be no hesitation in the serious nature of the message students receive regarding their personal accountability for ensuring patient safety.
Clearly defined medication competency curriculum threads addressing safety-related knowledge, skills, and attitudes need to be identified across all semesters in the program. Additionally, there are intentions to explore if nationally standardized National Council Licensure Examination (NCLEX) preparation exams (such as ATI) given at the end of each semester may be augmented with items to measure benchmarks for student medication calculation competencies, with increasingly complex problems progressing across the program. This is an area with potential for enhanced data collection locally and nationally.
Strategies that were drawn upon in the implementation of DA at the UTHCSCA School of Nursing included building knowledge and skills through self-paced online modules, faculty CEU incentives, student class expectations, local champions, math tutors, administrative support, and feedback of positive calculation accuracy outcomes. Medication calculation process consistencies (system competency) were improved as all clinical courses now formally teach and require students to use DA (with the exception of obstetrical nursing, in which students do not administer medications). Both students and faculty report improved medication confidence, competency, and value for a consistent, non-memory-based, universally applicable, practice process. Stronger methodology to quantify these reported outcomes is needed, moving forward. Barriers encountered during the implementation process included skepticism of the evidence, reticence of some faculty and students to change, comfort with past knowledge and skills, inconsistent reinforcement of DA in some courses, gaps in student application opportunities due to course sequencing, competition for content time, and limited accountability for full participation.
UTHSCSA School of Nursing faculty modeled lifelong learning and organizational leadership for quality and safety by collaborating to assure use of evidence-based practice across the School as a means of addressing the human factor of medication calculation errors. They supported students' accountability for individual practice and their development as nursing professionals through self-directed learning, engagement in DA evaluation, and input to build a safer healthcare system. This process has unified curricular focus, and it represented the first time in which faculty competency with a particular evidence-based ability was addressed directly and formally. It has established a new faculty competency standard, initiated a process for implementing system-wide change, illuminated barriers, and created a more cohesive community of learning in the School. It also supports the mission of the University to use evidence to drive quality outcomes, and to engage and involve stakeholders. Beginning in Summer 2010, the School of Nursing's Continuing Education Department incorporated the DA CEU modules into its Registered Nurse Refresher Course. Having received very positive reviews from the participants ("wish I had learned DA years ago," "I feel more comfortable with IVs and conversions than I thought I would"), the Department Director has recently shared the modules with a collaborating partner in a neighboring city. Clinical sites are also able to access the modules for staff development, upon request.
A knowledge translation model, coupled with faculty competency standards and sound online educational strategy, was used to drive the movement of evidence-based best practice from knowledge into action. This has demonstrated the potential for enhancing system competency to support the building of a climate of safety. Ongoing quality improvement benchmarking further demonstrates the critical nature of educational decisions related to implementation of curricula. Current evidence, faculty competencies, course-to-course articulation, deliberate teaching strategies, learner engagement in improvement, and a shared vision of the need for maximum student competency to impact future client outcomes are aspects that are required to effect rapid, measurable change and provide a template for future replication.
Change is challenging for all who are involved, and it is seldom perfect in process and/or outcome. As faculty determine how to continue to address student formation and their assumption of the demonstrated value of lifelong learning, it is necessary also to wrestle with how the process is modeled. There are further opportunities within this realm. At the UTHSCSA School of Nursing, it was learned that a model for effecting systemic change, sustained focus by champions, ongoing faculty committee support, and easy continual access to online learning modules presenting evidence-based practice can together be effective in responding to the IOM imperative of enhancing patient safety through stronger nurse competency and confidence with medication calculations. A link has also been identified between the QSEN safety competencies and student development that is now able to be addressed more fully in the School's undergraduate curriculum.
Future work to be undertaken includes quantitative evaluation of students' actual (as opposed to perceived/self-reported) calculation competency with DA, addition of enhanced mechanisms for affecting systemic change, and a broader look at how DA fits within the overall medication delivery process.
References
Agency for Healthcare Research and Quality. (2001). Translating Research Into Practice (TRIP)-II Fact Sheet. Retrieved from http://www.ahrq.gov/research/trip2fac.htm
American Association of Colleges of Nursing. (2008). The essentials of baccalaureate education for professional nursing practice. Washington, DC: Author. Retrieved from http://www.aacn.nche.edu/education/pdf/baccessentials08.pdf
American Nurses Association. (2007). Medication errors and syringe safety are top concerns for nurses according to new national survey. Retrieved from http://www.nursingworld.org/FunctionalMenuCategories/MediaResources/PressReleases/2007/SyringeSafetyStudy.aspx
Billings, D. M., & Connors, H. R. (n.d.). Best practices in online learning. In The living book of teaching and learning. New York, NY: National League for Nursing. Retrieved from http://www.electronicvision.com/nln/chapter02/
Billings, D. M., & Halstead, J. A. (2009). Teaching in nursing: A guide for faculty (3rd ed.). St. Louis, MO: Saunders.
Blank, F. S. J., Tobin, J., Macomber, S., Jaouen, M., Dinola, M., & Visintainer, P. (2009). A "back to basics" approach to reduce ED medication errors. Journal of Emergency Nursing, 37(2), 141-147. doi:10.1016/j.jen.2009.11.026
Boucher, D. (2007, June). Use of dimensional analysis to reduce medication errors in EMS. Maine EMS I/C News. Retrieved from http://www.vaniotis.com/jacky/Dimensional%20Analysis.htm
Brennan, T. A., Leape, L. L., Laird, N. M., Hebert, L., Localio, A. R., Lawthers, A. G. , ... Hiatt, H. H. (1991). Incidence of adverse events and negligence in hospitalized patients – Results of the Harvard Medical Practice Study I. New England Journal of Medicine, 324(6), 370-376. doi:10.1056/NEJM199102073240604
Craig, G. P. (1997). The effectiveness of dimensional analysis as a problem-solving method for medication calculations from the nursing student perspective (Doctoral dissertation). Retrieved from http://escholarshare.drake.edu/bitstream/handle/2092/461/dd1997gpc001.pdf
Cronenwett, L., Sherwood, G., Barnsteiner, J., Disch, J., Johnson, J., Mitchell, P., ... & Warren, J. (2007). Quality and safety education for nurses. Nursing Outlook, 55(3), 122-131. doi:10.1016/j.outlook.2007.02.006
Fleming, N. D., & Mills, C. (1992). Helping students understand how they learn. The Teaching Professor, 7(4).
Greenfield, S., Whelan, B., & Cohn, E. (2006). Use of dimensional analysis to reduce medication errors. Journal of Nursing Education, 45(2), 91-94.
Greiner, A. C., & Knebel, E. (Eds.). (2003). Health professions education: A bridge to quality. Washington, DC: The National Academies Press. Retrieved from http://www.nap.edu/openbook.php?isbn=0309087236
Institute of Medicine. (2006). Preventing medication errors. Retrieved from http://www.iom.edu/~/media/Files/Report%2520Files/2006/Preventing-Medication-Errors-Quality-Chasm-Series/medicationerrorsnew.pdf
Kohn, L. T., Corrigan, J. M., & Donaldson, M. (Eds.). (1999). To err is human: Building a safer health system. Washington, DC: The National Academies Press.
Kolb, D. A. (1984). Experiential learning: Experience as the source of learning and development. Englewood Cliffs, NJ: Prentice-Hall.
Landrigan, C. P., Parry, G. J., Bones, C. B., Hackbarth, A. D., Phil, M., Goldmann, D. A., & Sharek, P. J. (2010). Temporal trends in rates of patient harm resulting from medical care. New England Journal of Medicine, 363(22), 2124-2134. doi:10.1056/NEJMsa1004404
Leonard, M. (2010). Patient safety and quality improvement: Medial errors and adverse events. Pediatrics in Review, 31(4), 151-158. doi:10.1542/pir.31-4-151
McMullan, M., Jones, R., & Lea, S. (2010). Patient safety: Numerical and skills and drug calculation abilities of nursing students and registered nurses. Journal of Advanced Nursing, 66(4), 891-899. doi:10.1111/j.1365-2648.2010.05258.x
Phillips, J., Beam, S., Brinker, A., Holquist, C., Honig, P., Lee, L. Y., & Pamer, C. (2001). Retrospective analysis of mortalities associated with medication error. American Journal of Health System Pharmacy, 58(19), 1835-1841.
Quality and Safety Education for Nurses. (2011). Competency KSAs (Pre-Licensure). Retrieved from www.qsen.org/competencies/pre-licensure-ksas/
Rice, J., & Bell, M. (2005). Using dimensional analysis to improve drug dosage calculation ability. Journal of Nursing Education, 44(7), 315-318.
Rosswurm, M. A., & Larrabee, J. H. (1999). A model for change to evidence-based practice. Journal of Nursing Scholarship, 31(4), 317-322. doi:10.1111/j.1547-5069.1999.tb00510.x
Schlesselman, L. S. (2011). 10 strategies to reduce medication errors. Retrieved from https://secure.pharmacytimes.com/lessons/200809-01.asp
Schuster, M. A., McGlynn, E. A., & Brook, R. H. (1998). How good is the quality of health care in the United States? Milbank Quarterly, 76(4), 517-563. doi:10.1111/1468-0009.00105
Thomas, E. J., Studdert, D. M., Newhouse, J. P., Zbar, B. I. W., Howard, K. M., Williams, E. J., & Brennan, T. A. (1999). Costs of medical injuries in Utah and Colorado. Inquiry, 36(3), 255-264. Retrieved from JSTOR database. (29772835)
Wright, K. (2010). Do calculation errors by nurses cause medication errors in clinical practice? A literature review. Nurse Education Today, 30(1), 85-97. doi:10.1016/j.nedt.2009.06.009